What is the flu?
We’ll often hear people say they have the flu anytime the get sick with nasal congestion, aches, and a low-grade fever. Sometimes it is hard to differentiate the common cold from the flu. So what is the real deal on the flu?
The flu is an infection caused by the influenza virus. We’ll discuss a little more about what the flu virus is, its characteristics, and the illness it causes in this post. You can read about the flu shot (immunization) here.
The word ‘influenza’ comes from the Italian ‘influentia’ (influence) due to an ancient belief the sudden onset of flu epidemics were due to the the influence of some extraterrestrial force.
When we talk about the ‘flu’ we could be talking about the flu as an illness or the flu as a virus.
The ‘flu’ as an illness
The flu is an illness characterized by these symptoms:
- Fever, usually rapid onset
- Malaise (really tired, fatigued)
- Myalgias (muscle aches)
- Headache
- Pharyngitis (sore throat)
- Non-productive cough (you aren’t coughing anything up)
- Absence of coryza (runny nose) – this helps separate it clinically from the common cold
- Kids may also have:
- gastrointestinal symptoms (abdominal pain, vomiting)
- ear infections (otitis media)
- croup
- myositis
The flu, though it seems bad and is very uncomfortable, is generally a mild & self-limited illness. However, there can be complications from the illness. Complications of influenza virus infection include:
- Primary viral pneumonia (influenza)
- Secondary viral pneumonia (caused by a different virus such as adenovirus)
- Secondary bacterial pneumonia
- Myositis and cardiac involvement
- Neurological syndromes, e.g. Guillan-Barre Syndrome
- Encephalopathy
- Encephalitis
- Reye’s Syndrome – this is why kids shouldn’t take aspirin for a fever
Allen Smith contracted the Swine Flu and had quite an extreme response. Fortunately, thanks to high-dose vitamin C, he is alive and well today. Here is a video of his story:
How does flu cause the illness?
The influenza virus can establish infection of the upper and lower respiratory tract.
The systemic symptoms noted with the flu are due to the inflammatory response the body mounts due to the infection. Part of this response involves the release of interferon and lymphokine. The interferon and cell-mediated responses (NK and T cells) are very important for both immune resolution of the virus and immunopathogenesis. Some medications (tylenol, anti-inflammatory medications such as ibuprofen) that we take to control symptoms of the flu can inhibit this inflammatory & immune response and can reduce the body’s ability to fight off the virus. This is why I often do not recommend medications to treat fever under most circumstances.
There is a layer of epithelial cells that line the entire respiratory tract from the tip of the nose to the bottom of the lungs. They have specialized functions such as cilia that help move particles out of these areas and mucus secretion. The local symptoms, such as coughing, are due to damage to these specialized epithelial cells. These cells are important for optimal function and protection.
People who have the flu are at higher risk for bacterial superinfection because of the loss of natural barriers and the induction of bacterial adhesion to the epithelial cells due to the damage stated above. Antibody production appears to be important for future protection against infection and is specific for epitopes on HA and NA. We’ll talk more about this stuff below but you can also read more about it in the flu shot post.
How is the flu spread?
The flu is generally spread through the air by aerosolized, infected particles from the coughs or sneezes of infected patients. The airborne aerosols are thought to be the most common mode of transmission but we don’t know for sure. Influenza can be spread directly by contact with nasal secretions or bird droppings. The infected material can be deposited on surfaces such as door knobs.
The influenza virus is inactivated by sunlight (UV light), disinfectants, and detergents. Since detergents (soap) are effective against the influenza virus frequent handwashing may help reduce the risk of infection.
Infected persons begin shedding new virus particles the day before symptoms develop and shed new viruses for 5-7 days. Thus, they are contagious BEFORE they have symptoms.
How do we diagnose the flu?
First, not everyone needs to be tested. One of the primary reasons to test is that some physicians may prescribe anti-flu medications if you have had symptoms for less than 48 hours.
Rapid Influenza Diagnostic Tests (RIDTs)
These tests can help diagnose flu in patients who have signs and symptoms consistent with the flu. They can also help determine if outbreaks of respiratory illness are due to influenza (i.e., nursing homes). In general, rapid diagnostic testing for influenza should be done when the results will affect clinical decision making.
These tests can detect Influenza A & Influenza B. They take less than 30 minutes to perform and are accomplished by obtaining a nasal swab, wash, or aspirate. They may or may not differentiate the type of flu present but they don’t give detail about the strain (H1N1, H3N5, etc).
The false negative rate (when the test is negative but you really do have it) is relatively high but false positives can also occur.
These tests are immunoassays in order to detect the flu virus.
Virus Isolation
We can isolate influenza flu virus particles from respiratory secretions. We obtain a direct aspirate, gargles, or nasal washings. These samples are then examined by immunofluorescence of the exfoliated cells. They can also be inoculated in cell cultures or embryonated eggs.
Serum antibodies can be assessed by hemagglutination inhibition.
Diagnostic Methods
- Cell culture in primary monkey kidney cells for the presence of virus
- Hemadsorption to infected cells for the presence of hemadsorbing virus
- Antibody inhibition of hemadsorption for the presence of influenza, type, and strain
- Immunofluorescence, ELISA – Influenza virus antigens in respiratory secretions or cell culture
- Hemagglutination – presence of virus in secretions
- Hemagglutination inhibition (HI) – type and strain of influenza virus
- Serology: this form of testing is not recommended
Epidemiology
Influenza A is essentially an avian virus that has “recently’ crossed into mammals. Birds have the greatest number and range of influenza strains. Avian hemagglutinins sometimes appear in pig, human, and horse influenza strains.
About every 10-15 years a major new pandemic strains appears in humans, with a totally new HA and sometimes NA as well (antigenic shift). The new variant causes a major epidemic around the world (pandemic).
This strain undergoes minor changes (antigenic drift) every 2 years. This is probably driven by selective antibody pressure in the populations of infected humans.
Influenza A Evolution
- 1874 – H3N2
- 1890 H2N2 Pandemic
- 1902 – H3N2
- 1918 – H1N1 Pandemic
- 1933 – H1N1 First strain isolated
- 1947 – H1N1 Variation detected (antigenic shift)
- 1957 – H2N2 “Asian” flu pandemic
- 1968 – H3N2 “Hong Kong” flu pandemic
- 1977 – H1N1 “Swine” flu, Fort Dix, non-epidemic
- 1978 – H1N1 “Russian” flu epidemic
- 1983 – H3N2 “Philippines” flu pandemic
- 2000 – H3N2 “Sidney” flu epidemic & H1N1
Influenza B epidemics occurs in Influenza A ‘off’ years. Influenza B often co-circulates with Influenza A.
This constant antigenic change down the years means that previous flu vaccines are not effective against new strains. Thus, new flu shots are formulated on a regular basis. New influenza strains spread rapidly in daycare centers and schools and in places where people crowd together. Influenza epidemics may cause significant economic losses due to high morbidity and mortality rates.
Because another devastating pandemic strain (1918 pandemic killed 20-40 million people worldwide) may appear any time, the World Health Organization (WHO) maintains worldwide surveillance of influenza strains and makes predictions of suitable strains for vaccine production.
Small clusters of human infections with avian influenza type A (H5N1) and (H9N2) occurred in Hong in 1997-98 from contact with infected fowl. So far, none of these strains have become established in humans. However, the incidence caused worldwide concern about the possible emergence of new “killer” influenza virus strains and intensified influenza research and vigilance programs.
The flu as a virus:
Viruses are bits of RNA or DNA that are able to incorporate into cells and cause damage or alter the function of those cells. They are not technically living and are unable to replicate or reproduce on their own.
Virus structure:

Influenza is a negative ss-RNA genome of 8 separate segments, nucleoprotein (NP) and 3 polymerases. The ‘negative’ ss-RNA means that the virus genome is RNA in a single-strand form (ss) which encodes for mRNA.
The nucleocapsid is enclosed within an outer lipoprotein envelope which carries 2 protruding spikes. One spike is a box-shaped protein called the neuraminidase (NA) which has properties of an enzyme (as the -ase at the end of the name suggests). The function of the neuraminidase (NA) assists with movement of the influenza virus particles through the respiratory tract mucus and the release of the virus particles from the infected cells. There are 9 major antigenic types of NA (1-9).
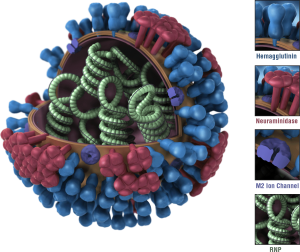
Thus, H1N1 virus has HA type 1 and NA type 1.
Inside the virus envelope is an ill-defined antigenic protein called the Matrix Protein (MP). The lipoprotein envelope of the influenza virus makes the virion susceptible to heat, drying, detergents, and solvents.
Classification: Orthomyxoviridae
The classification of influenza is done on the basis of antigenicity of NP and HA into 3 main groups:
- Influenza A: HA & NA undergo minor and occasionally major changes. It can be the cause of epidemics and pandemics
- Influenza B: Relatively slow changes in time. Influenza B is only seen in humans. It can be the cause of epidemics.
- Influenza C: Uncommon, filamentous strain that is only seen in humans. Typically there are only sporadic cases of Influenza C.
Influenza is named by this nomenclature: A/Singapore/6/86/H1N1
This means: Influenza A / Town where it was first isolated / Number of isolates / Year it was isolated / Major type of HA & NA
How does the virus replicate?
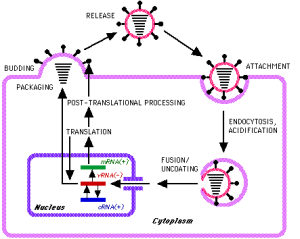
When the virus is making new viral proteins they are translated from transcribed mRNA. New viral RNA is encased in the capsid protein which is then transported to cell membrane batches which have been modified by viral Matrix Protein (MP) and the HA and NA spikes membrane proteins. The underlying MP acts as a homing device, so to speak, for the nucleocapsids.
The new virus particles are formed inside the cell and are released from the cell by a process called budding. The cell does not die in this process. At least not initially.
The influenza virus has a segmented genome structure. This means that there are ‘chunks’ of RNA that can act, or be acted upon, separately and can reorganize their structure when a cell is infected with 2 different viral strains. This structure greatly increases the recombination potential and contributes to the rapid development of new virus strains in nature. The reassortment process is duplicated in the lab for making flu immunization strains.
Avian and human strains combining in pigs in the Far East are the main source of new virulent human strains. This is why we (Americans) go to Asia when we are looking for which influenza strains may be spreading to the US for selection in the flu shot.
Emergence of new influenza virus strains
New influenza virus type A strains arise by recombination between human and animal strains as stated above. This is called ‘antigenic shift‘. In contrast, type B influenza virus strains arise by point mutation which is called ‘antigenic drift‘.
Read about the Flu Shot
Read about how to prevent & treat the flu







